The Active Risk Control (ARC) Toolkit
Current practice in healthcare risk management is supported by many tools for risk assessment (understanding problems), but none for risk control (solving problems). The results: a failure to improve safety, and a waste of the investment made in risk assessment. The Active Risk Control (ARC) Toolkit, available for free, fills this void with a systematic, structured approach to risk control.
Here is the ARC Toolkit:
ARC-Toolkit-2013-Version-1.3.3
The updated Train-the-Trainer orientation to the Toolkit can be found here:
ARC-Toolkit- Train-the-Trainer Version-1.3.3
A brief presentation introducing the ARC Toolkit can be downloaded here:
https://drive.google.com/file/d/0BxOvkwYtUvpJUnlWUXo4ejN1Ymc/view
————————————————————————————————————————
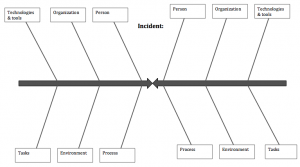
The Lovebug Diagram
Have you ever used a Fishbone / Ishikawa Diagram to assess an adverse event or near miss? If so, you only got half the picture. The Lovebug Diagram will help you explore both what went wrong and what went right. In addition to its role as incdent investigation tool, the Lovebug Diagram can also be used as a structured approach to Force-Field Analysis. Force-field analysis examines the forces for and against a planned change (or the status quo) and can be used for applications such as change management, risk control analysis, or community-based participatory research.
Two Lovebug Diagram templates are provided here. The first focuses on patient safety incident analysis and is structured around the SEIPS model by Carayon, et al. (as seen above). The second focuses on organizational change management and is built around Weiner’s Theory of Organizational Readiness for Change. Any number of other frameworks could be used for either purpose, and I encourage you to find the one that works best for you.
A Lovebug Diagram with category headings based on the SEIPS Model
Lovebug Diagram – Theory of Org Readiness for Change
Publications on the Lovebug Diagram:
Card AJ. A new tool for hazard analysis and force field analysis: The Lovebug Diagram. Clin Risk 2013;00:00. Available from: http://cri.sagepub.com/content/19/4-5/87.abstract An earlier version of the paper is also available at: tinyurl.com/LovebugDiagram
————————————————————————————————————————
The Generating Options for Active Risk Control (GO-ARC) Technique
You’ve completed your risk assessment. You understand the problem. Now what?
Whether you used root cause analysis (RCA), failure mode and effects analysis (FMEA), structured what-if technique, or any other widely-used risk assessment tool, you are now left entirely to your own devices when it comes to designing solutions.
The Generating Options for Active Risk Control (GO-ARC) Technique is a structured brainstorming technique that will help you generate a broader and deeper set of potential solutions (risk control options) to choose from.
Using five brainstorming prompts, you will come up with ways of applying five different risk control strategies to the risk at hand. The prompts are presented one-by-one, along with a brief just-in-time training element consisting of a definition and illustrative examples.
This tool is a fast and easy way of making sure you don’t always fall back on the same weak risk controls that caused your problem in the first place.
A spreadsheet-based version of the GO-ARC Technique is provided here:
Publications on the GO-ARC Technique:
Card, AJ, Ward JR, & Clarkson PJ. Generating Options for Active Risk Control (GO-ARC): Introducing a Novel Technique. Journal for Healthcare Quality. 2013;doi: 10.1111/jhq.12017. Available from: http://onlinelibrary.wiley.com/doi/10.1111/jhq.12017/abstract
The Risk Curve Approach to Risk Evaluation / Risk Scoring
The traditional “risk matrix” approach to risk evaluation / risk scoring assumes that each risk will be associated with exactly one level of likelihood and exactly one level of impact. In healthcare and public health, there are actually very few risks that fit this profile. More often, a risk can lead to multiple levels of impact, each with its own likelihood of occurrence.
In these cases, any single likelihood-impact pairing you choose will necessarily be wrong and misleading–defeating the whole point of the exercise.
One way to deal with this is to extend the logic of the risk matrix by simply mapping out the level of likelihood associated with each level of impact (constructing a risk curve).
This (verr brief) presentation explains how to use the risk curve approach:
We first proposed the risk curve approach here: Risk scoring with the risk curve approach
Card AJ, Ward JR, & Clarkson PJ. Trust-Level Risk Evaluation and Risk Control Guidance in the NHS East of England. Risk Analysis. 2014;34(8), 1471-1481. [Published online ahead of print: Dec 2013]; DOI: 10.1111/risa.12159.
Also available from: https://www.researchgate.net/publication/259348245_Trust-Level_Risk_Evaluation_and_Risk_Control_Guidance_in_the_NHS_East_of_England
Other publications describing this approach include:
Card AJ. Real Risks Have Curves: A New Way of Using the Risk Matrix. Risk Watch. Summer 2015, 19-23.
Shope DW, Assoc. Eds:, Allman CJ, Card AJ, Siders C, Sine DM, eds. Enterprise Risk Management Playbook. 2nd ed. American Society for Healthcare Risk Management; 2020. https://www.ashrm.org/enterprise-risk-management-playbook-second-edition
The Structured What-If Technique (SWIFT)
The structured what-if technique (SWIFT) is a structured brainstorming technique that can be used for risk assessment. It is similar to failure mode and effects analysis (FMEA), except for two things:
1. It does not go into the same level of detail on the process steps to be risk assessed. It is, therefore, considerably faster. (It may take only 1/3 the amount of time required for an FMEA.) The advice I have heard for SWIFT is to map out your process or system using no more than 10 steps / components.
2. It uses a structured brainstorming approach. You apply a series of brainstorming prompts to each step of the process or component of the system you are assessing. Each prompt helps you consider different types of hazards that might be present in the system.
SWIFT can be used by itself, or as part of a staged approach. In the staged approach, SWIFT is used as a screening tool, allowing you to quickly identify risks in more straightforward components of your system, while also identifying the components of your system that would benefit from the use of a more detail-oriented risk assessment technique, such as FMEA or fault tree analysis.
Unlike the three techniques above (The ARC Toolkit, the Lovebug Diagram and the GO-ARC Technique), the Structured What-If Technique is not my invention. But I have been working to popularize it in the healthcare industry because it is faster and more engaging than FMEA (probably the most-used prospective risk assessment technique in healthcare). I hope that will help reduce some of the barriers that prevent healthcare organizations from taking a more proactive approach to patient safety improvement.
A SWIFT template is provided below.
Publications on SWIFT:
Card AJ, Ward J, Clarkson PJ. Beyond FMEA: The Structured What-If Technique (SWIFT). Journal of Healthcare Risk Management. 2012;31(4), 23-29. Available from: http://onlinelibrary.wiley.com/doi/10.1002/jhrm.20101/abstract
Or from: https://www.academia.edu/1269393/Beyond_FMEA_The_Structured_What-If_Technique_SWIFT_
For more on SWIFT, I recommend:
Ward J, Clarkson J, Buckle P, Berman J, Lim R, Jun T. Prospective Hazard Analysis: Tailoring Prospective Methods To A Healthcare Context. 2010. Available from: http://www.webcitation.org/6KZ0Y4R8E
At the end of this (quite long) report is the Prospective Hazard Analysis (PHA) Toolkit, which provides a practical approach to using PHA techniques in healthcare organizations. SWIFT is one of the tools included, along with several others.
Potts HW, Anderson JE, Colligan L, Leech P, Davis S, Berman J. Assessing the validity of prospective hazard analysis methods: a comparison of two techniques. BMC Health Serv Res 2014;14:41. Available from: http://www.biomedcentral.com/1472-6963/14/41
This paper is an updated and peer-reviewed version of one of the ‘gray literature’ reports cited in my SWIFT paper. It makes an important contribution because it is one of very few comparative effectiveness studies of healthcare risk management tools.